Key results
across patient, care delivery, finance, sales, marketing, and HR
auto-refreshed and validated daily for enterprise-wide access
tracked across revenue cycle, engagement, and workforce efficiency
through optimized RCM workflows and real-time process visibility
About the Client
The client is a prominent US-based healthcare enablement organization offering cost-containment, clinical advocacy, and benefits optimization solutions. As they scaled services across multiple domains, the lack of centralized data visibility hindered operational efficiency and decision-making across functions.
Key Challenges
Siloed Systems - Disconnected data from Accuity, QuickBooks, NetSuite, ESO Office, and Microsoft Access
Manual Reporting Bottlenecks - Time-consuming processes delayed insights and operational agility
Limited Cross-Functional Visibility - Gaps in patient care metrics, revenue performance, and workforce analytics
Inconsistent Data Quality - Lack of automated validation and standardized definitions for KPIs
Our Approach
- Designed a Cloud-Native Analytics Architecture on Snowflake (AWS) for scalability and performance
- Developed modular data pipelines to integrate, clean, and standardize clinical, financial, and operational datasets
- Implemented role-based access and validation frameworks to ensure secure, accurate, and real-time reporting
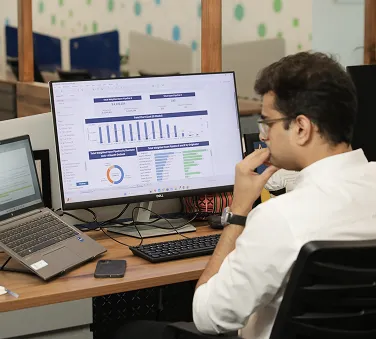
- Deployed Tableau dashboards for self-service insights across teams
- Introduced predictive models to drive proactive care and financial planning
Implemented Solution
Data Engineering & Warehousing
- Unified data ingestion from Accuity, QuickBooks, NetSuite, ESO Office, and legacy Microsoft Access databases
- Developed curated data marts for core domains: Revenue Cycle, Patient Engagement, Sales & BD, Marketing, and Workforce
- Enabled daily automated refresh with QA checks and audit trails for compliance
Business Intelligence
- Patient Experience: Drop-off analysis, NPS tracking, channel effectiveness
- Revenue Cycle (RCM): AR aging, payer-level variance, denial code patterns, claim volume trends
- Sales & Business Development: Lead pipeline, conversion funnel, rep productivity
- Marketing: Campaign ROI, cost-per-lead (CPL), attribution by channel
- Workforce & HR: Attrition trends, diversity metrics, hiring velocity, retention benchmarks
ML based Predictive Modeling
- Revenue Forecasting: Modeled claim cycle timelines to predict monthly revenue flow
- Patient Churn Prediction: Identified disengagement risks using care history and behavioral signals
- Claims Anomaly Detection: Flagged high-risk claims with early denial indicators using ML-based pattern analysis
Technologies Used